CLOSE![]()
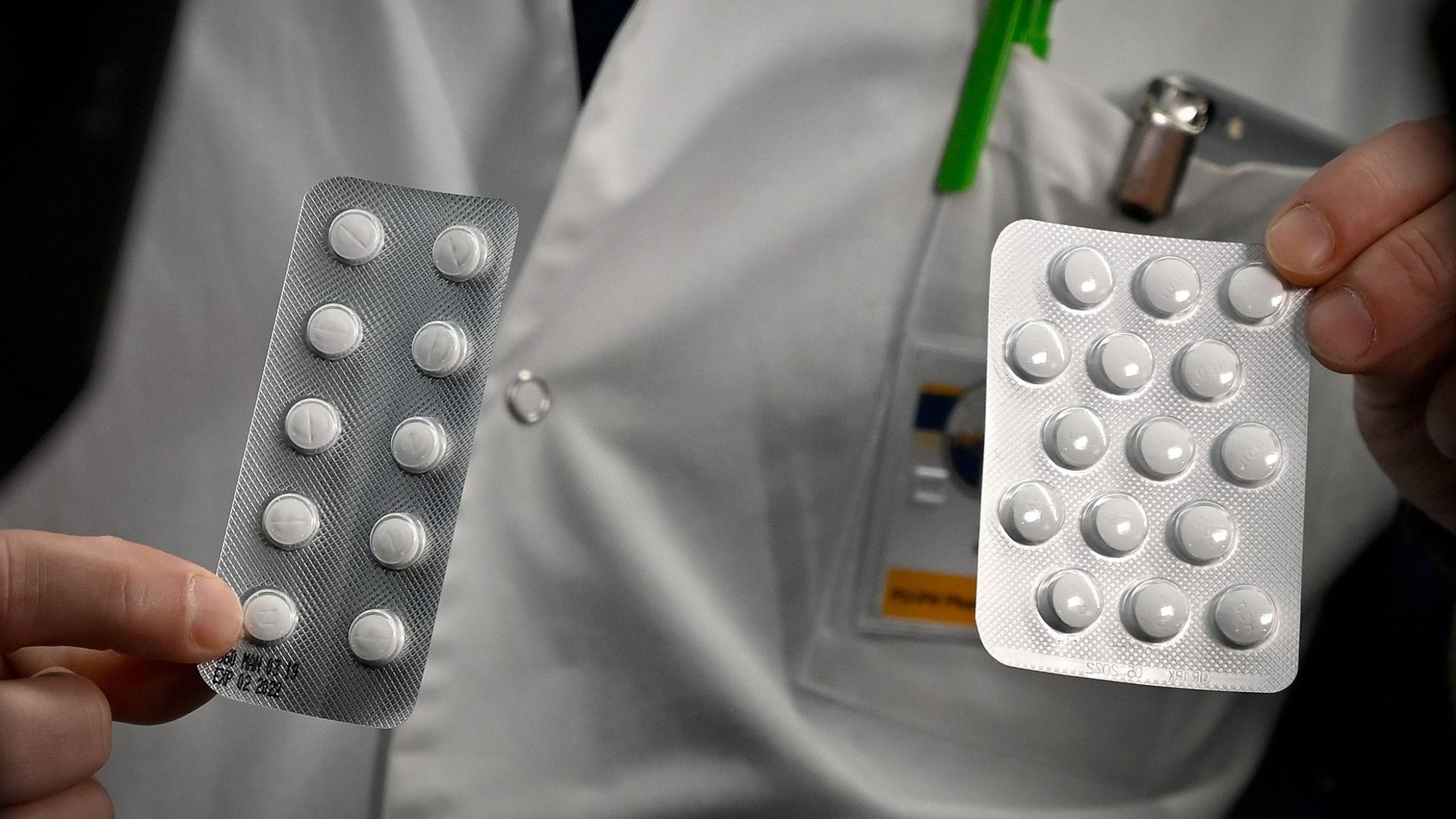
Dr. Raymond Woosley says anti-malarial drugs like chloroquine can cause subtle heart changes and increase a person’s risk of developing arrhythmia.
USA TODAY
A double-blind research study of a drug touted by President Donald Trump early on to treat coronavirus found it to be so dangerous at high doses the trial was shut down after six days.
The study on chloroquine, conducted in Brazil, found one-quarter of the patients taking the anti-malaria medication developed potentially deadly changes in the electrical system regulatingtheir heartbeats. While a small and imperfect study, it highlights the compelling need for more rigorous data.
Doctors in the United States have seen such heart issues with chloroquine and a similar but less toxic drug, an anti-inflammatory called hydroxychloroquine. Some medical systems are no longer using either to treat COVID-19, even if they initially tried it. Others use them only with careful monitoring.
The Infectious Diseases Society of America guidelines panel on Saturday recommended patients hospitalized with COVID-19 be given chloroquine or hydroxychloroquine in the context of a clinical trial.
Rajesh Gandhi, an infectious diseases physician at Massachusetts General Hospital and professor at Harvard Medical School, was on the IDSA guidelines panel that created the guidelines published over the weekend.
“The IDSA guidelines panel concluded that the data so far for hydroxychloroquine and chloroquine is insufficient to be either for or against it,” Gandhi said. “We don’t know that it doesn’t work or that it works.”
More: In the midst of furious coronavirus work, scientists must also socially distance in the lab
The evaluation found studies showing potentially dangerous changes in the electrical patterns of some patients’ hearts, as well as gastrointestinal side effects. It acknowledged there is a “knowledge gap” about what is known, making clinical trials crucial.
“The guidelines are a living document, we’ll continue to update as we get more data,” Gandhi said.
Despite the lack of certainty surrounding the efficacy of the drugs, Trump continues to promote them. He first heralded both chloroquine and hydroxychloroquine as possible cures for COVID-19 in briefings in March and has done so repeatedly, as recently as Tuesday, during a White House media event with people who’ve recovered from COVID-19.
Trump asked if they’d taken “the Hydroxy” and said, “I actually haven’t heard a bad story” about the drug. He went on to indicate that while Americans understood its importance, the news media did not.
Some researchers worry the president’s focus on the drugs has put too high a priority on exploring their use over other, potentially more promising drugs.
And despite Trump’s assertions, medical scientists remain unconvinced of the drugs’ safety or effectiveness.
“Like many other medical centers that were desperate to come up with something to help people who had COVID-19 seriously enough to require hospitalization, we originally started using hydroxychloroquine,” said Daniel Kaul, a professor of infectious disease at the University of Michigan school of medicine.
After several weeks, they saw no clear benefits for patients but very clear side effects, including a change in the electrical patterns in some patients’ hearts similar to the findings of the Brazilian study. While a patient experiences no symptoms,the shifting patterns show up on an electrocardiogram and are a warning sign of a potentially fatal heart arrhythmia.
In the last week of March, the University of Michigan stopped giving hydroxychloroquine except in the context of carefully controlled clinical drug trials.
“It caused us to take a long step back and look very carefully at the data,” Kaul said. “When we analyzed it, it was so flawed as to be uninterpretable and no evidence of benefit so we stopped using it.”
Many medical centers, including the University of California, San Francisco, Harvard, the Mayo Clinic and the University of Washington are not prescribing either drug for COVID-19 outside of clinical studies or in very specialized cases.
“It was reasonable, based on data we had a week ago, to use hydroxychloroquine,” said Andrew Badley, an infectious disease specialist at the Mayo Clinic in Rochester, Minnesota. “We now have the Brazilian trial, and there are other trials that have been submitted for review. As those results become available, we may or may not need to modify our thinking.”
Experts noted information about what drugs are effective is constantly changing and treatment options available at individual medical centers can vary widely. Some, including in hard-hit New York, continue to use the drug on critically ill patients.
At Stony Brook Medicine, a medical system on Long Island, New York, that includes multiple hospitals and clinics, doctors originally gave most COVID-19 patients both hydroxychloroquine and an antibiotic, azithromycin, based on early data from a tiny French study. They stopped giving azithromycin early on because they observed heart issues.
“Now we give hydroxychloroquine to most (COVID-19) patients but discourage it in elderly patients that have significant cardiac disease. We also monitor patients constantly,” said Bettina Fries, infection diseases division chief at Stony Brook Medicine.
With more than 400 COVID-19 patients in the system, they haven’t had the luxury to set up more than a few clinical trials, she added.
“We had to pull every physician out of every clinic just to deal with the surge,” Fries said. Finding the labor simply to enroll patients in a clinical trial, a very time-consuming and bureaucratic process, simply wasn’t possible.
Brazilian study stopped at Day Six
The study from Brazil published on Saturday was among the first larger and more rigorous released on chloroquine. However, it included only 81 patients, lacked placebo controls and was a rushed preprint, so it cannot be used as a sole source for treatment decisions.
Patients also were given the antibiotic azithromycin and most got an antiviral treatment, oseltamivir, both of which can cause the same electrical issues in the heart muscle, noted Kome Gbinigie, a researcher at the Center for Evidence Based Medicine at Oxford University’s Nuffield Department of Primary Care Health Services in England. Gbinigie co-authored a review of chloroquine and hydroxychloroquine as treatments for COVID-19 that appeared April 7 in the British Journal of General Practice.
Despite these confounding factors, the Brazilian findings offer “a cautionary tale,” said George Daley, dean of Harvard Medical School.
“It’s such an object lesson for the need for clinical trials to take precedence over gut feeling and intuition,” he said. “It teaches us that there are real risks to drugs and it’s dangerous to advocate for an unproven therapy when you might not be taking the risks and benefits into account.”
The trial was conducted at a public hospital in the Brazilian city of Manaus and posted on Saturday to medRxiv, an online server for medical articles that have not yet gone through the peer-review process.
Beginning March 23, half the participants were given a high dose of 600 milligrams of chloroquine two times a day. Half were given a low dose of 450 milligrams twice a day for the first day and then a single dose each day. The patients also received azithromycin and another antibiotic.
On day six of the trial, 11 patients had died and a quarter of those getting the higher dosage showed abnormal electrical activity in the heart.
The researchers closed the high dose part of the study and moved all remaining patients to the low dose regimen. In their paper, they wrote the high dose of chloroquine “was not sufficiently safe to warrant continuation of that particular study arm.”
Like much related to COVID-19, the study comes with many caveats. It was not peer-reviewed and not subject to the stringent publication requirements of a major scientific journal. It was, however, double-blinded and randomized, meaning neither the patients nor the doctors knew who was getting what dose and patients receiving either the low or high dose were randomly selected.
It is the first of many expected studies looking at the effectiveness of both chloroquine and hydroxychloroquine.
History casts doubt on effectiveness
It’s long been known that chloroquine and the similar drug hydroxychloroquine – both which have been used in much lower doses to treat malaria – can affect electrical impulses in the heart.
“This particular compound has over 40 known different side effects,” said John Scott, the chair of the department of pharmacology at the University of Washington in Seattle. “If you affect the electrical signaling of the heart, you’re in trouble.”
Many infectious disease doctors doubtthe effectiveness of chloroquine and hydroxychloroquine for treating COVID-19, said Otto Yang, a professor of infectious disease at the University of California, Los Angeles.
Their reasoning is based on history. While multiple lab studies have found chloroquine to show good activity against viruses including HIV and influenza, “all controlled clinical trials treating these diseases failed,” he said.
When it comes to treating the virus that causes COVID-19, Yang said, “I see no reason why it would be different for SARS-CoV-2.”
Autoplay
Show Thumbnails
Show Captions
Read or Share this story: https://www.usatoday.com/story/news/2020/04/15/coronavirus-chloroquine-test-halted-drug/2983129001/